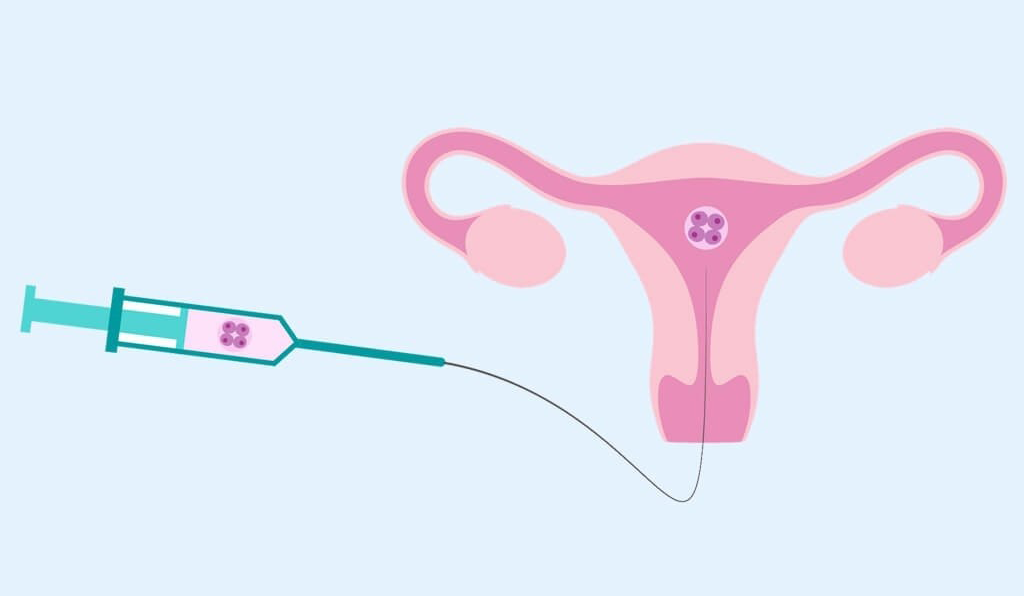
Intrauterine insemination IUI treatment is a type of artificial insemination in which a physician places sperm obtained from a male within a woman’s uterus to aid in conception.
IUI aims to increase the likelihood of conception by addressing some infertility issues and putting sperm close to mature eggs after Ovulation.
Table of Contents
When Donated Sperm Is Required To Achieve Conception, Iui Is Routinely Utilised.
IUI procedures can include fertility testing by International Fertility Group, ovulation induction medicine, choosing a sperm donor, and sperm placement surgery. Infection from the technique, which is uncommon, and multiple pregnancies (twins or more), if assisted reproduction medication is utilised, are risks associated with IUI.
One of the first methods of assisted reproduction that is frequently suggested by a doctor is IUI. In addition to helping those with unexplained infertility, endometriosis, or cervical mucus problems, it can also aid same-sex couples and is frequently utilized when the husband is experiencing low sperm count or poor sperm motility. The procedure’s minimally intrusive nature appealed to me. Healthy sperm are simply positioned as close to the Oviduct as possible, providing them a slight advantage as they travel toward the egg.
The IUI procedure was challenging to navigate, as it is with anything related to infertility. I soon engaged my physical, emotional, and monetary resources in something I didn’t fully understand. I was very curious: What happens?
The Evaluation
My husband had his sperm examined to determine the concentration, motility, and morphology of his tiny guys on Day 3 of my cycle. I also had blood tests done to assess my hormone levels. A medication-assisted IUI or a natural IUI were our two choices. The former involves using fertility medicines to encourage the maturation of several follicles (usually two or three) and increase the likelihood of conception; the latter does not (so only one egg is released). We decided on a natural IUI as it was my first reproductive treatment and we didn’t want anything too invasive.
Step 2: Cycle Observation
On Day 10, I started a daily cycle check at my clinic. Every day for a week, I had to show there early—between 8 and 8:30 a.m.—for blood testing and an internal ultrasound. I couldn’t help but feel like a pincushion, despite the fact that I knew the procedure would offer my doctors information on how my hormonal changes and follicles were growing. By Day 17, a developed follicle was prepared to ovulate, my nurse informed me. (I thought this was gruelling, so it was about time.)
Step 3: Fire the Trigger
The first hormone shot I had ever had was my trigger shot. I received hCG, a pregnancy hormone that promotes follicular maturation and prompts ovulation within 36 hours. To help timing insemination, doctors provide this hormone; they want men to be waiting for the developed egg. Needles don’t bother me, but I’m used to receiving them in my arm rather than my abdomen. I know I flinched even though the trigger shot didn’t hurt because it felt so strange.
Pre-Procedure, Step Four
We arrived just at clinic on Day 18 at 7 a.m. for IUI day. It would be an understatement to say we were anxious because neither of us knew what to anticipate. Was the procedure painful? Would your husband be permitted to join me in the room? Additionally, there was a great deal of expectation because we were counting on the IUI to be successful.
My husband generated a sample of semen after I performed my customary bloodwork and internal ultrasound. We were instructed to come back to the clinic around midday so the andrologist would have time to “wash” his swimming trunks. (Eggs washing is the process that separates sperm from semen and eliminates the “tadpoles” of inferior sperm.)
It felt strange to have to wait after our early-morning appointment before the surgery. We found ourselves in Toronto at around 8 a.m. without anything to do for the next four hours. We were at a loss for what to do for a long because we both wanted our IUI to be over. We bought groceries, fueled up our car with petrol, then treated ourselves to breakfast. We now chuckle about how bizarre everything is.
On the Ultrasound Room in Step Five.
I sat on the examination table and put my feet in the saddle when I returned to the ultrasound room. We were asked to confirm that the data on a vial of my husband’s sperm matched ours after being shown the vial. I can still hear myself saying, “I almost certainly hope so,” but all I could do was laugh aloud. Such a silly, yet significant, request. Prior to responding “Yes,” I believe I read the content 100 times. The doctor then requested me to lie down and placed a speculum inside my vagina.
The Implantation is Step Six.
The doctor put the tube into my vaginal and my cervix while the technician conducted an external ultrasound on me. She put the catheter into the cervical canal and directed it toward the top of my uterus the right Fallopian tube using the ultrasonography screen as her guide (which I carefully observed during the process) (the side with the mature follicle). She used the catheter to inject my uterus with my husband’s sperm before telling me to remain seated for a while. The entire operation took approximately 60 to 90 seconds.
The Sensation of IUI
The IUI procedure itself was unpleasant and painful, but it didn’t hurt. The catheter was inserted, and the sensation was similar to a quick, painful pinch. According to Ari Baratz, a fertility expert at the Create Fertility Centre in Toronto, “most women relate it to a Pap test.”
The worst aspect of the treatment was having to endure the dreaded “two-week wait.” Before your period, when all you can do is lounge around and fantasise about getting pregnant. It’s torture because there’s no way to tell if you’re pregnant at that point, but that’s all you can worry about.